Coronavirus hospitalizations are increasing in many rural and less populated areas that were previously relatively unaffected.
Doctors and health officials worry that infections will overwhelm small communities that have a short supply of medical resources.
“The 20% of the U.S. population that lives in rural areas consists of generally older individuals with more chronic conditions who are more likely to be under- or uninsured,” said Joanna Hart, MD, MSHP, an Assistant Professor of Medicine at the Perelman School of Medicine. “They are more likely to be experiencing poverty and have limited access to health care. Even before COVID-19, rural hospitals faced significant financial challenges and operational limitations. The volume and acuity of COVID-19 cases in those areas will quickly overwhelm the very limited resources of many rural communities.”
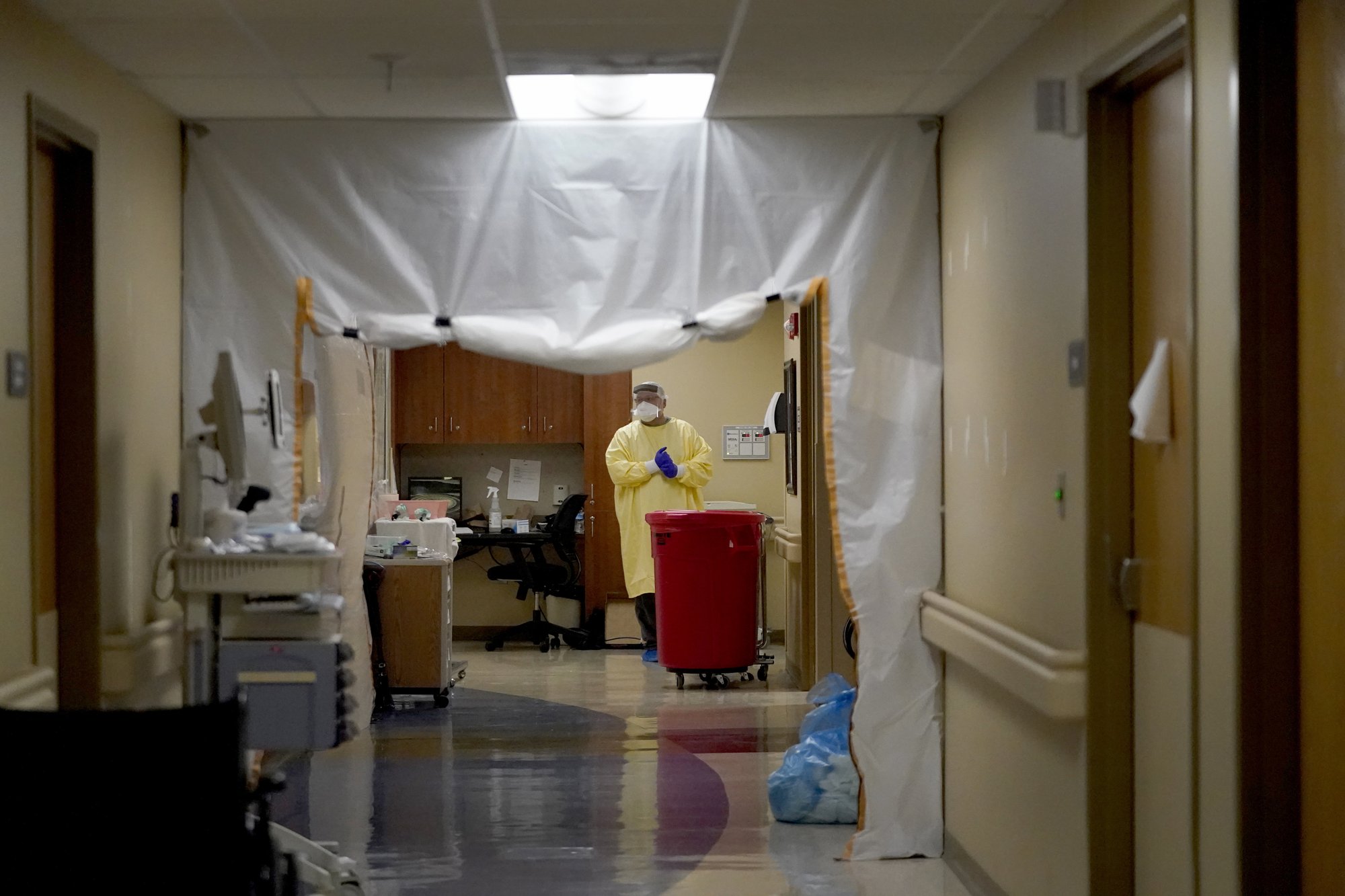
Many hospitals suffering from staffing shortages are putting out an appeal for anyone with health care experience, including retirees. Scotland County Hospital Chief Nursing officer, Elizabeth Guffey, said Nurses are working up to 24 extra hours each week.
In counties with just a few thousand people, the number of cases per capita can soar with even a small outbreak. “One or two people with infections can really cause a large impact when you have one grocery store or gas station,” said Misty Rudebusch, the Medical Director at a network of rural health clinics in South Dakota called Horizon Health Care. “There is such a ripple effect.”
These rural states don’t have the luxury of having multiple large hospitals in every city so they are relying on smaller hospitals with roughly six Doctors and 75 Nurses among 142 full-time staff, they can’t handle the increase in cases.
Another limiting factor amongst these rural states are the amount of open ICU beds. Doctors are calling surrounding hospitals asking to transfer patients to help free up beds or turning them away if they aren’t sick enough. They are also sending patients home, potentially with oxygen assistance, and having them call back if their condition gets worse.
Kootenai Health, a rural hospital in northern Idaho, said that the hospital is 99% full of patients needing medical or surgical care. “As we have been working to accommodate patients, several regional hospitals have either declined to accept transfers due to their own capacity/staffing, or they have been highly selective about which patients they can accommodate. For this reason, we are looking at hospitals beyond our normal transfer area to see what is available.”
According to the National Rural Health Association, Nearly half of all rural hospitals were operating at a financial loss prior to the COVID-19 outbreak and are now facing catastrophic cash shortages. The rate of rural hospital closures, already at crisis levels pre-COVID-19, will soon escalate to cataclysmic rates.
Even as outbreaks threaten to spiral out of control, Doctors and health officials said they are struggling to convince people of the seriousness of this virus.
“The more rural you get, the more disdainful people are, the more doubting and skeptical they are about the whole COVID story,” said Dr. William Schaffner, a Vanderbilt University School of Medicine professor of preventive medicine and an infectious disease specialist.
West River Health Services in Hettinger, North Dakota, CEO Matthew Shahan said he has seen more people wearing masks in recent weeks, particularly friends and family of those who’ve gotten sick. “It’s going to take a lot of communication from everyone at all levels of the state to get this done.”